School of Public Health
Sickle Cell Disease
What is it? |
On this page |
|---|---|
|
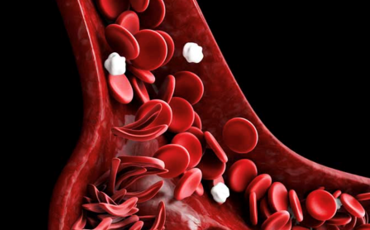
Sickle cell disease (SCD) is a group of inherited red blood cell disorders. In SCD, the red blood cells become hard and sticky and look like a C-shaped farm tool called a “sickle.” People with SCD can live full lives and enjoy most of the activities that other people do. If you have SCD, it’s important to learn how to stay as healthy as possible. Click on any of the links below to learn more.
|
Causes
SCD is a genetic condition that is present at birth. It is inherited when a child receives two genes - one from each parent - that code for abnormal hemoglobin. DiagnosisSCD is diagnosed with a simple blood test. In children born in the United States, it most often is found at birth during routine newborn screening tests at the hospital. In addition, SCD can be diagnosed while the baby is in the womb. Diagnostic tests before the baby is born can check for chromosomal or genetic abnormalities in the baby. Because children with SCD are at an increased risk of infection and other health problems, early diagnosis and treatment are important. Talk to your doctor to find out how to get tested and to explain the results after testing. TreatmentSpecific Treatments to Prevent SCD Complications SCD is a disease that worsens over time. Treatments are available that can prevent complications and lengthen the lives of those who have this condition. These treatment options and their effects can be different for each person, depending on the symptoms and severity of their disease. It is important to understand the benefits and risks of each treatment option. Currently, the FDA has approved four treatments for SCD[1].
Several other treatments and therapies for SCD have recently been developed that are still undergoing clinical trials and thus have not yet been approved by the FDA. Specific treatments to cure SCD Curative treatments are available for SCD, but they are not widely available yet.
It is important for SCD patients to be seen in specialty clinics, where doctors (hematologists) and other staff are trained specifically in SCD. Unfortunately, not everyone with SCD has access to a specialty clinic. These are the SCD treatment centers in TN. All of them take TennCare and all treat patients from a wide geographical area. Click on these center to learn more. Memphis
Nashville
Knoxville
|