UofM Magazine

When early studies on COVID-19 started to emerge last winter, Brandt Pence immediately began making parallels between his work and the virus’ behavior.
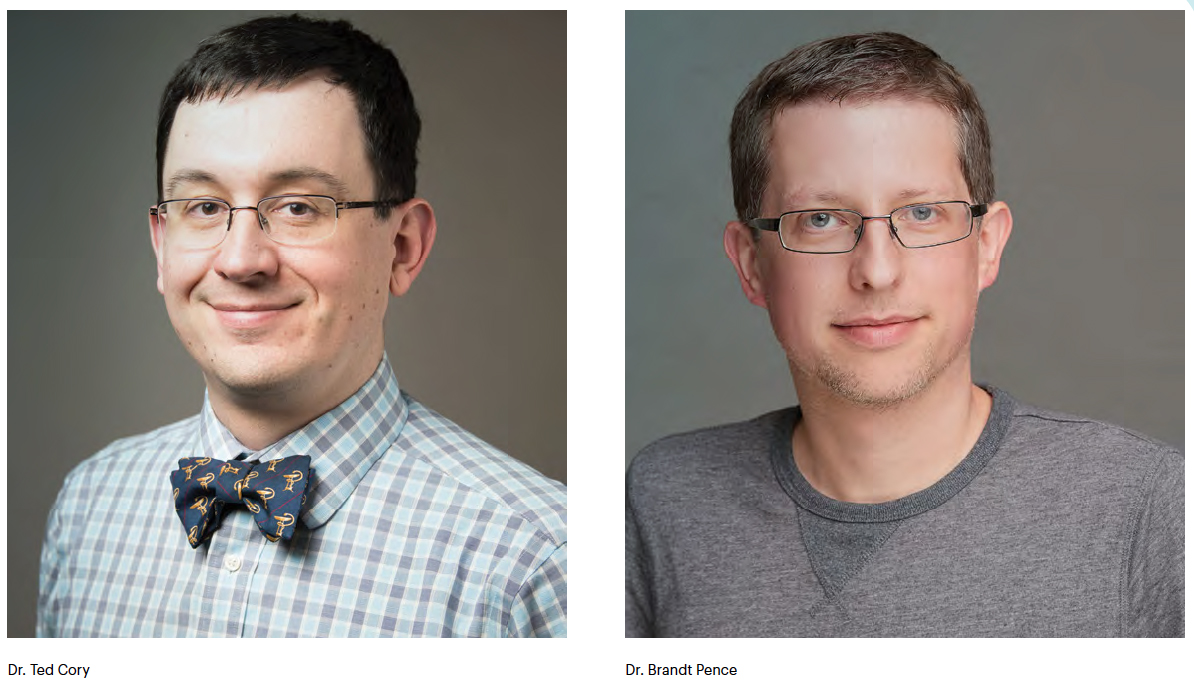
Pence is an assistant professor of nutrition in the College of Health Sciences at the UofM. His research is focused on aging and its impact on the immune system, with a specific interest in how changes in metabolism impact inflammatory and cellular functions of certain white blood cells.
“It was apparent fairly quickly to me there were potential links between what I was doing and COVID-19,” said Pence, whose work is supported by the American Heart Association, the American College of Sports Medicine, the University of Washington Nathan Shock Center and internal awards from the UofM.
“Exploring what was being shown in some of these observational early studies with specific immune responses that I study, that was really where I started to be able to draw some comparisons and interest in digging deeper.”
In June, Pence published a paper on the potential connections between his area of research and severe COVID-19 cases. He also began doing specific research on the virus in his own lab and in collaboration with the Regional Biocontainment Lab at the University of Tennessee Health Science Center.
The work of Pence, and many other researchers like him, is critical in the fight against the coronavirus. It will continue to take experimentation, collaboration and support within health sciences to better understand the very important relationship between aging, the immune system and the severity of COVID-19 cases in order to develop therapies to combat the virus.
ARE MONOCYTES THE KEY?
Pence first began working with monocytes, a white blood cell that helps fight infection, as an undergrad at Purdue University. He assisted in a lab focused on their role in the immune system, particularly as they impact age-related diseases.
His June paper — “Severe COVID-19 and aging: are monocytes the key?” — surmised that monocytes may be the key driver in a phenomenon called cytokine storm, an overreaction within the immune system causing more harm than good. Many of the most severe cases of COVID-19 exhibit high levels of cytokines, small proteins the body releases to trigger inflammation as a response to infection.
 “When cytokines are in excess, it can cause organ failure, tissue destruction and
things of that nature that ultimately can cause death,” Pence said. “We know that
monocytes, which produce cytokines as an early immune response, are floating around
in the blood at all times. In severe COVID-19 cases, they move into the lungs, start
pumping out a bunch of cytokines and that’s when we see the serious symptoms such
as acute respiratory distress syndrome, which has been noted in a lot of critical
cases.”
“When cytokines are in excess, it can cause organ failure, tissue destruction and
things of that nature that ultimately can cause death,” Pence said. “We know that
monocytes, which produce cytokines as an early immune response, are floating around
in the blood at all times. In severe COVID-19 cases, they move into the lungs, start
pumping out a bunch of cytokines and that’s when we see the serious symptoms such
as acute respiratory distress syndrome, which has been noted in a lot of critical
cases.”
Beyond the respiratory issues in COVID-19 patients, these cells are also directly related to the systemic effects. That includes the gastrointestinal and nervous systems and many organs outside of the lungs.
“Monocytes appear to be major players in causing these inflammatory responses that lead to tissue destruction and many of the main effects that cause severe COVID- 19,” said Pence. “While it’s not uncommon to see this with many diseases, it’s very important to understanding and assessing how to counteract COVID-19.”
THE IMMUNE RESPONSE TO COVID-19
Much of the focus on solving the pandemic has understandably revolved around the development of a vaccine. But even once a vaccine becomes readily available to the public, there are no guarantees to its level of effectiveness, especially for the population that is the most at risk for severe cases.
 “There’s a lot of progress being made with vaccines as several hundred are being developed,”
Pence said. “But at the same time, we know from other vaccines that older adults have
a higher tendency not to respond to them as well. So, understanding the immune response
to the virus is essential to developing therapies that can help overcome deficiencies
and lead to better outcomes overall.”
“There’s a lot of progress being made with vaccines as several hundred are being developed,”
Pence said. “But at the same time, we know from other vaccines that older adults have
a higher tendency not to respond to them as well. So, understanding the immune response
to the virus is essential to developing therapies that can help overcome deficiencies
and lead to better outcomes overall.”
Pence’s lab began studying the relationship between monocytes and COVID-19’s spike proteins, whose crown-like shape give coronavirus its name, last summer. They began by using purified versions of the proteins to stimulate monocytes and determine the level of inflammatory response in the lab.
“We found that it does cause a very large increase in the production of cytokines, and thus, massive inflammation,” Pence said. “Again, that isn’t particularly surprising as it’s something we saw with the original SARS virus and the MERS virus, which are closely related to what we’re dealing with now. But it’s nonetheless important to establish as a starting point.”
Pence’s lab took a deeper dive into this relationship by analyzing if spike proteins were causing metabolism changes in monocytes. Establishing this theory could play an important role in finding effective solutions to combating dire cases of COVID-19.
“This is one of the things that we started to look at that hadn’t really been looked at before,” Pence said. “We are seeing some early data showing there are changes in metabolism with monocytes that are similar to what you see when these cells are exposed to bacteria and things like that.
“This potentially opens up opportunities to look at therapeutics that are known to block some of these metabolic responses and might have efficacy in fighting the cytokine storm that can cause severe COVID-19 cases.”
COLLABORATION IS ESSENTIAL
Experts working together across many sectors of the health and science communities have been vital in the fight against COVID-19.
For example, Pence is unable to conduct research using the actual virus without access to a biocontainment lab. There are just 14 universities in the entire country with one of these facilities.
“There are not a lot of places in the United States that are approved to study a virus like this, so the vast majority of researchers don't have the ability to actually directly study the virus,” Pence said. “That is where collaboration among researchers and research facilities has become essential to understanding the virus and finding solutions. Fortunately, the scientific community is generally very collaborative.”
The University of Tennessee Health Science Center in Memphis is one of the few institutions with a Regional Biocontainment Laboratory. Pence began collaborating with UTHSC in the summer to conduct research using the live virus to analyze the immune response in whole organisms rather than relying on purified spike proteins.
Pence’s collaboration with the lab is just one of the many ways the UofM and UTHSC have partnered in the battle against COVID-19. The two institutions teamed up in a venture to secure CORNET grants allocated for COVID-19 research, an effort that yielded 23 research proposals. Pence and UTHSC’s Ted Cory were awarded a CORNET grant in July. They are collaborating to determine if senescent cells, which are increased during aging, have greater inflammatory responses to the virus.
The UofM also accessed University Clinical Health, a clinical practice affiliate of UTHSC, to provide testing for students returning to campus in the fall.
This level of cooperation, in Memphis and across the country, is paramount to saving lives. The same is true of the need for further growth in health sciences as communities navigate through and move past a pandemic.
A SURGE IN HEALTH SCIENCES?
The College of Health Sciences has consistently been one of the fastest-growing programs at the UofM in recent years. With nearly 1,700 declared majors and more than 50 full-time faculty and staff, the college projects to continue building rapidly.
CHS has added a handful of new programs with more expected in the near future at both the undergraduate and graduate levels. Additionally, research within the CHS is growing significantly with the hiring of scientific leaders receiving national and international recognition for their work.
 “Over the past five years, we have doubled in our number of declared majors, while
significantly expanding our research portfolio and laboratories,” said CHS dean Dr.
Richard Bloomer. “We are certainly moving forward and will continue to do our collective
best to provide a great education to our students.”
“Over the past five years, we have doubled in our number of declared majors, while
significantly expanding our research portfolio and laboratories,” said CHS dean Dr.
Richard Bloomer. “We are certainly moving forward and will continue to do our collective
best to provide a great education to our students.”
This growth and emphasis within the UofM’s CHS are representative of expected trends throughout the country. An aging population and an ever-evolving health care system are bringing about significant growth in health science careers. The U.S. Bureau of Labor Statistics projects 2.4 million new jobs in health care by 2026, a remarkably higher growth rate than the average of all other occupations.
There are no apparent positives to a pandemic. There may, however, be a silver lining considering the increased awareness in health sciences across the country.
“My hope is that we will see the interest continue to grow, not just here but all over the U.S. and the world,” Pence said. “Our population is growing older. Every year we are going to see people 65 and over, who tend the be the individuals that need the most health care, making up a greater percentage of our population. There will be continued demand for people in these fields, and I think there’s increasing awareness of how important it is.”
