Calendar & Curriculum

2023-24 Program Calendar
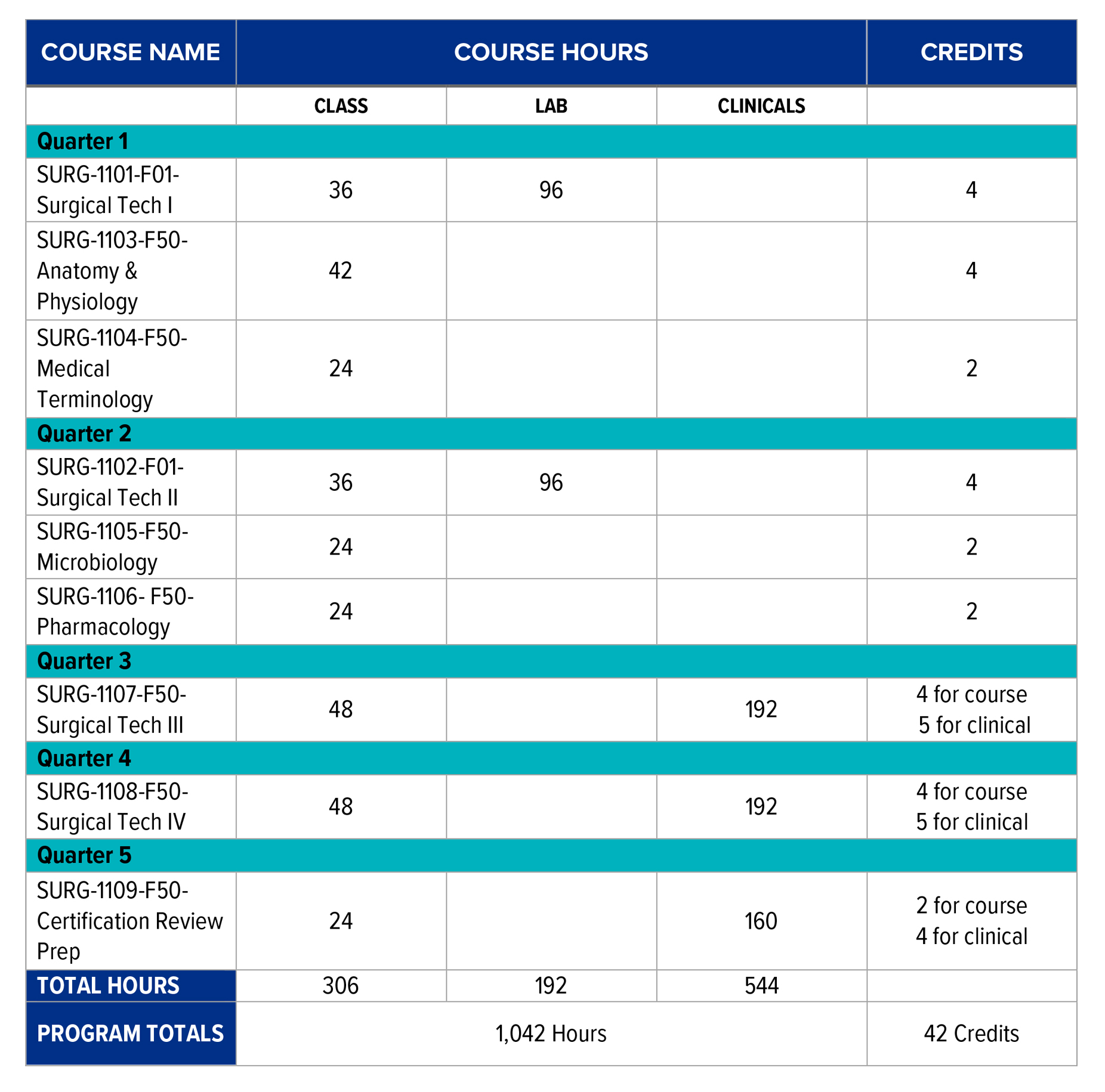
There are a total of four 12-week terms and one 10-week term. All coursework, except for the lab and clinical time, will be delivered through an online method.
Term I
- First day - Jan. 16, 2023
- Last day - April 9, 2023
- Break - April 10-16, 2023
Term II
- First day - April 17, 2023
- Last day - July 9, 2023
- Break - July 10-16, 2023
Term III
- First day - July 17, 2023
- Last day - Oct. 8, 2023
- Break - Oct. 9-15, 2023
Term IV
- First day - Oct. 16, 2023
- Break - Dec. 18, 2023 -Jan. 2, 2024
- Last day - Jan. 21, 2024
Term V
- First day - Jan. 22, 2024
- Last day/final day of program - April 1, 2024
Criteria for Completion & Graduation
Graduation Requirements
Students must finish all didactic courses as well as complete the required 120 clinical cases in order to graduate. Students are required to complete all courses with a grade of “C” or higher in all academic and clinical requirements contained within the program curriculum/syllabus in the sequence outlined. Each course is a prerequisite for subsequent courses and must be taken in the designated order.
The goals and objectives of the program correlate with the current Edition of the Core Curriculum for Surgical Technology. Once the curriculum and clinical requirements have been fulfilled, students are required to take the Certified Surgical Technologist Exam given by the NBSTSA.
*All students are required to sit for the certification exam given by the NBSTSA in order to graduate.
Grading Procedure
All students are expected to finish with a grade of "C" or higher in order to move on to the next course.
Grading Scale
- 90-100: A
- 80-89: B
- 70-79: C
- 60-69: D
Probation Procedure
A student may be placed on probation for any of the following reasons:
- Academic
- Attendance
- Behavior
- Clinical
If a student is placed on probation for any reason, they will receive a probation form directly from the Program Director. This form will include all details on what must be done in order to be taken off of probation and must be signed by the student. Failure to comply may result in dismissal from the program.
Clinical Case Requirements
To graduate from the University of Memphis Surgical Technology program, a total of 544 hours and 120 clinical cases must be completed that include a designated variety of specialized settings. Students will track and account for their cases using an official spreadsheet provided by the program. Only cases having a preceptor evaluation form completed and signed by the preceptor will be logged on the spreadsheet. Students should log their cases daily and always have the current log available for referral. This enables students to know what they need for clinical cases in the event their schedule must be modified because the originally assigned case is no longer viable.
A. General Surgery Cases
Students must complete a minimum of 30 cases in general surgery; 20 which must be performed in the First Scrub Role. The remaining 10 cases may be performed in either the First or Second Scrub Role. *See below for description of Roles.
B. Specialty Cases
Students must complete a minimum of 90 cases in various surgical specialties, excluding general surgery.
- A minimum of 60 cases must be performed in the First Scrub Role and evenly distributed
between a minimum of four surgical specialties.
- A minimum of 10 cases in the First Scrub Role must be completed in each of the required minimum of four surgical specialties (40 cases total required).
- The additional 20 cases in the First Scrub Role may be distributed amongst any one surgical specialty or multiple surgical specialties.
- The remaining 30 surgical specialty cases may be performed in any surgical specialty either in the First or Second Scrub Role.
C. Optional Surgical Specialties
- Diagnostic endoscopy cases and vaginal delivery cases are not mandatory. However, up to 10 diagnostic endoscopic cases and five vaginal delivery cases can be counted toward the maximum number of Second Scrub Role cases.
- Diagnostic endoscopy cases must be documented in the category of "Diagnostic Endoscopy", rather than by specialty.
- Vaginal delivery cases must be documented in the category of "Labor & Delivery'' rather than in the OB/GYN specialty.
D. Counting Cases
- Cases will be counted and documented according to surgical specialty in one of the following categories: General Surgery, Cardiothoracic, ENT, Eye, GU, Neuro, Ob-Gyn, Oral/Maxillofacial, Orthopedics, Peripheral Vascular, Plastics, Procurement/Transplant, Diagnostic Endoscopy, or Labor & Delivery.
- Examples of counting cases:
-
- Trauma patient requires a splenectomy and repair of a Lefort I fracture. Two cases can be counted and documented since the splenectomy is a general surgery specialty and repair of LeFort I is an oral-maxillofacial surgical specialty.
- Patient requires a breast biopsy followed by mastectomy. It is one pathology, breast cancer, and the specialty is general surgery. Therefore, it is counted and documented as one case.
- Endoscopic cases that convert to an open case will be counted as only one case. For example: a laparoscopic cholecystectomy converted to an open cholecystectomy.
- Case experience in the Second Scrub Role is not mandatory.
First and Second Scrub Role & Observation
First Scrub Role
The student surgical technologist shall perform the following duties during any given surgical procedure with proficiency. The following list is provided to identify the items that must be completed in order to document a case in the First Scrub Role. A student not meeting the five criteria below cannot count the case in the First Scrub Role and the case must be documented in the Second Scrub Role or Observation Role.
- Verify supplies and equipment needed for the surgical procedure.
- Set up the sterile field with instruments, supplies, equipment, medication(s) and Solutions needed for the procedure.
- Perform counts with the circulator prior to the procedure and before the incision is closed.
- Pass instruments and supplies to the sterile surgical team members during the procedure.
- Maintain sterile technique as measured by recognized breaks in technique and demonstrate
knowledge of how to correct with appropriate technique.
Second Scrub Role
The Second Scrub Role is defined as the student who is at the sterile field who has not met all criteria for the First Scrub Role, but actively participates in the surgical procedure by performing one or more of the following:
- Sponging
- Suctioning
- Cutting suture
- Holding retractors
- Manipulating endoscopic camera
Observation Role
The Observation Role is defined as the student who is in the operating room performing roles that do not meet the criteria for the First or Second Scrub Role. These observation cases are not to be included in the required case count, but must be documented.

